Joint Hypermobility Syndrome: When Flexibility Becomes a Problem
Learn about joint hypermobility syndrome—when overly flexible joints cause pain and instability. Understand symptoms, diagnosis, and management strategies.
By Joint Pain Authority Team
Key Takeaways
- Joint hypermobility means joints move beyond the normal range of motion
- Hypermobility becomes a “syndrome” when it causes symptoms like pain and instability
- It’s a spectrum—from benign flexibility to connective tissue disorders like EDS
- Treatment focuses on strengthening muscles to stabilize joints
- Many hypermobile people can live active, healthy lives with proper management
- Diagnosis is clinical—there’s no blood test or imaging that confirms it
Being flexible is usually considered a good thing. Dancers, gymnasts, and yoga practitioners often prize their range of motion. But for some people, joints that bend too far cause more problems than benefits—chronic pain, frequent injuries, and joints that feel unstable.
If your joints have always been “too flexible” and you experience pain or injuries others don’t, you may have joint hypermobility syndrome.
What Is Joint Hypermobility?
Defining Hypermobility
Joint hypermobility means your joints move beyond what’s considered the normal range of motion. Your ligaments (the tissues connecting bones) are more lax than usual, allowing greater flexibility.
Examples:
- Bending your thumb to touch your forearm
- Hyperextending your elbows or knees beyond straight
- Bending forward to place palms flat on the floor with straight knees
- Fingers that bend backward significantly
Hypermobility vs. Hypermobility Syndrome
Simple hypermobility:
- Joints are flexible but don’t cause problems
- Very common, especially in children and young women
- Often an advantage in certain activities
- No treatment needed
Hypermobility Spectrum Disorder (HSD):
- Hypermobility plus symptoms
- Joint pain, instability, or recurrent injuries
- Symptoms affect daily life
- Treatment focuses on management
Hypermobile Ehlers-Danlos Syndrome (hEDS):
- More severe end of the spectrum
- Specific diagnostic criteria (2017 criteria)
- Often involves multiple body systems
- Family history common
The Spectrum
Think of hypermobility as existing on a spectrum:
Asymptomatic flexibility → Hypermobility spectrum disorder → hEDS → Rarer EDS types
Most hypermobile people fall somewhere in the middle—experiencing some symptoms but managing well with appropriate care.
Who Is Affected?
Prevalence
- About 10-20% of the general population has some degree of hypermobility
- Much more common in children (flexibility naturally decreases with age)
- 2-3 times more common in women than men
- More common in certain ethnic groups (Asian, African descent)
- Hypermobility syndrome (with symptoms) affects about 3% of the population
Risk Factors
- Female sex: Hormones affect connective tissue laxity
- Family history: Strong genetic component
- Ethnicity: Some populations have higher rates
- Age: Hypermobility decreases with age but symptoms may persist
Signs and Symptoms
The Beighton Score
The Beighton score is a simple clinical tool to assess hypermobility. One point for each of the following (max 9 points):
- Pinky fingers: Can bend back beyond 90 degrees (1 point each hand)
- Thumbs: Can bend to touch the forearm (1 point each hand)
- Elbows: Hyperextend beyond straight (1 point each arm)
- Knees: Hyperextend beyond straight (1 point each leg)
- Forward bend: Palms can rest flat on floor with knees straight (1 point)
Score interpretation:
- ≥4/9 in adults (≥5/9 in children): Suggests generalized hypermobility
- Score alone doesn’t diagnose a syndrome—symptoms must also be present
Common Symptoms
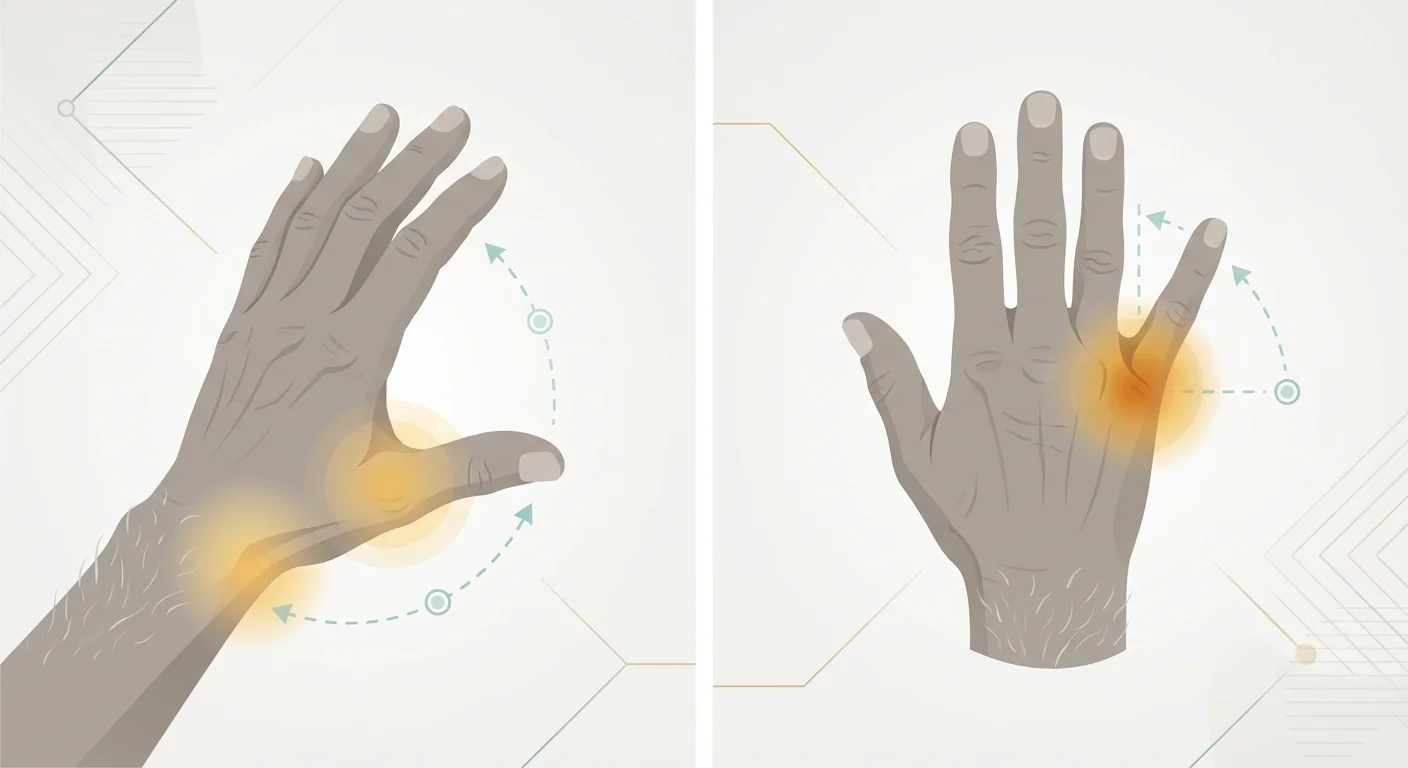
Joint-related:
- Joint pain (often widespread)
- Recurrent joint dislocations or subluxations
- Early-onset osteoarthritis
- Frequent sprains and strains
- Joints that “pop” or “click”
- Feeling that joints are unstable or “give out”
Muscle-related:
- Muscle fatigue and pain
- Muscle cramps
- Reduced muscle strength
- Feeling of heaviness in limbs
Other common features:
- Chronic fatigue
- Headaches
- Digestive issues (IBS-like symptoms)
- Dizziness when standing (dysautonomia)
- Anxiety
- Poor proprioception (sense of body position)
- Soft, stretchy, or fragile skin
- Easy bruising
- Slow wound healing
The Triad
Many people with hypermobility syndrome experience a common triad:
- Joint hypermobility with pain and instability
- Autonomic dysfunction (POTS, dizziness)
- Mast cell activation (allergies, reactions, skin issues)
This overlap is increasingly recognized by specialists.
Diagnosis
Why Diagnosis Can Be Challenging
- No definitive lab test
- Symptoms overlap with many other conditions
- Many doctors aren’t familiar with hypermobility spectrum disorders
- Symptoms may be dismissed as “just being flexible”
- Criteria have changed over time
How Diagnosis Is Made
Clinical evaluation:
- Beighton score assessment
- Joint examination
- Medical and family history
- Symptom evaluation
For hypermobile EDS specifically (2017 criteria):
- Generalized joint hypermobility (Beighton score)
- Two or more of:
- Systemic features (soft skin, hernias, etc.)
- Family history
- Musculoskeletal complications
- Exclusion of other causes
Ruling out other conditions:
- Autoimmune diseases
- Other connective tissue disorders
- Marfan syndrome
- Other EDS types (some have genetic tests)
Who Can Diagnose
- Rheumatologists
- Geneticists (especially for EDS)
- Physiatrists (physical medicine doctors)
- Some knowledgeable primary care doctors
Treatment and Management
The Foundation: Strengthening and Stability
The most important treatment for hypermobility is building muscle strength to compensate for ligament laxity.
Why this works:
- Ligaments can’t be “tightened”
- Strong muscles actively stabilize joints
- Better muscle control improves proprioception
- Prevents injuries by supporting vulnerable joints
Exercise approach:
- Low-impact activities initially
- Focus on stability and control
- Progress gradually (hypermobile joints are injury-prone)
- Water-based exercise often well-tolerated
- Pilates and specific physiotherapy protocols helpful
- Avoid end-range stretching (you don’t need more flexibility!)
Physical Therapy
Work with a therapist who understands hypermobility:
Key focus areas:
- Core stability
- Proprioceptive training (balance, body awareness)
- Joint-specific strengthening
- Posture correction
- Pacing strategies for fatigue
What to avoid:
- Pushing joints to their full range
- High-impact activities initially
- Exercises that stress already-unstable joints
- Generic stretching programs
Pain Management
Non-medication approaches:
- TENS units
- Heat/ice as appropriate
- Massage (gentle)
- Acupuncture (may help some people)
- Pacing activities to avoid boom-bust cycles
Medications:
- NSAIDs for acute pain (long-term use problematic)
- Acetaminophen for chronic pain
- Low-dose antidepressants (help with chronic pain and sleep)
- Avoid opioids if possible (don’t address the underlying issue)
Joint Protection
Splinting and bracing:
- Can provide stability for specific joints
- Especially helpful during activities
- Should not replace strengthening
- Avoid overuse (muscles can weaken)
Activity modification:
- Avoid positions that hyperextend joints
- Use good body mechanics
- Take breaks during repetitive activities
- Listen to your body’s signals
Managing Other Symptoms
Fatigue:
- Pacing (most important strategy)
- Sleep hygiene
- Treating underlying dysautonomia if present
Dysautonomia (POTS):
- Increased salt and fluid intake
- Compression stockings
- Gradual exercise progression
- Medications if needed (under specialist care)
Anxiety:
- Cognitive-behavioral therapy
- Understanding that anxiety is common with chronic pain
- Treatment of underlying physical symptoms helps
Living Well with Hypermobility
Mindset Shifts
Helpful perspectives:
- “My joints are different, not defective”
- Focus on what you can do, not limitations
- Strength training is treatment, not optional
- Pacing isn’t giving in—it’s strategic
- Progress may be slow but is possible
Building Your Support Team
- Physical therapist experienced with hypermobility
- Doctor who understands the condition
- Mental health support if needed
- Online communities for shared experiences
Activities to Consider
Often well-tolerated:
- Swimming and water exercise
- Cycling (low impact)
- Pilates (with knowledgeable instructor)
- Walking (with appropriate footwear)
- Strength training (controlled, progressive)
Approach with caution:
- Yoga (avoid end-range stretching)
- Running (depends on individual)
- Contact sports (injury risk)
- Activities with high joint stress
Frequently Asked Questions
Is joint hypermobility the same as Ehlers-Danlos syndrome?
Not exactly. Joint hypermobility is a feature that exists on a spectrum. Hypermobile EDS (hEDS) is at the more severe end of that spectrum and has specific diagnostic criteria beyond just being flexible. Most hypermobile people don’t have EDS, but hEDS is the most common type of EDS.
Will my hypermobility get worse with age?
The flexibility itself typically decreases with age (joints stiffen). However, accumulated joint damage can cause increasing symptoms over time. Proper management helps minimize long-term complications.
Can hypermobility be cured?
No, the underlying connective tissue laxity is genetic and can’t be changed. However, symptoms can be managed very effectively with strengthening, pacing, and other strategies. Many people with hypermobility live full, active lives.
Should I avoid stretching?
You should avoid aggressive stretching or pushing to your full range of motion. You already have plenty of flexibility—what you need is stability. Gentle movement is fine, but you don’t need to “improve” your flexibility.
Is hypermobility related to autoimmune diseases?
Hypermobility itself is not autoimmune. However, some people with hypermobility spectrum disorders have conditions like POTS or mast cell activation that involve immune system dysfunction. True autoimmune diseases are separate conditions.
Can children be diagnosed with hypermobility syndrome?
Children are naturally more flexible, making diagnosis more complex. A Beighton score of 6/9 or higher is typically needed to consider a child hypermobile. Diagnosis usually focuses on whether symptoms are present and affecting function, not just flexibility.
Looking for more information on joint conditions? Explore our guides on fibromyalgia and joint pain or visit our conditions hub.
Last medically reviewed: February 2025
Medical Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. If you suspect you have joint hypermobility syndrome, please consult a healthcare provider experienced in this condition.
Enjoyed this article?
Get more insights like this delivered to your inbox weekly.
Join 10,000+ readers. No spam.