Fluoroscopy-Guided Injection: A Technical Overview
An in-depth technical guide to fluoroscopy-guided knee injections. Understand the technology, accuracy rates, procedure details, and why imaging guidance matters for treatment outcomes.
By JPA Medical Team
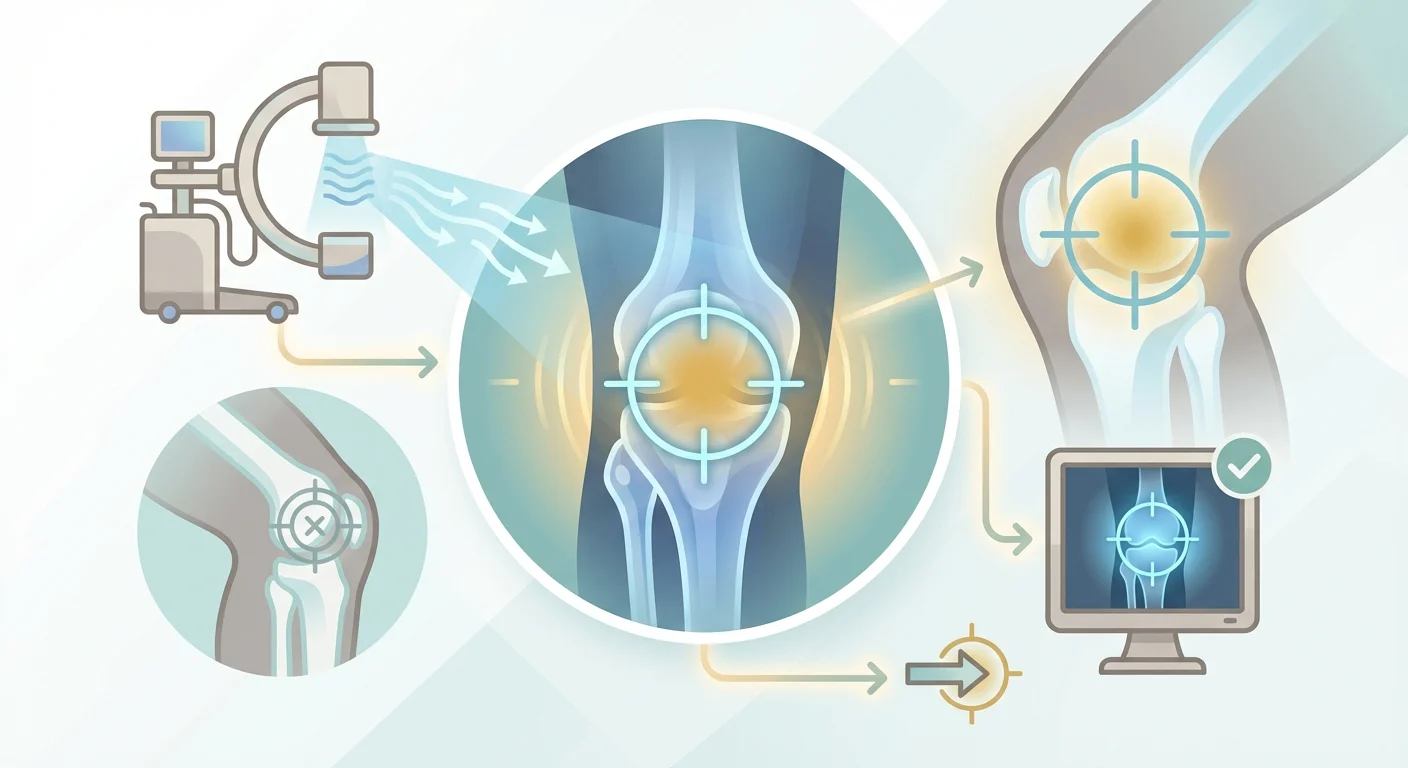
Technical Overview: Fluoroscopy-Guided Knee Injections
This guide provides detailed information about fluoroscopy-guided injection technology—what it is, how it works, and why it produces better outcomes than blind injection techniques.
Part 1: What Is Fluoroscopy?
Definition
Fluoroscopy is a real-time X-ray imaging technique that allows physicians to visualize internal structures during procedures. Unlike static X-rays, fluoroscopy provides continuous imaging, similar to an X-ray “movie.”
How It Works
Basic Components:
- X-ray source - Generates radiation beam
- Image intensifier - Converts X-rays to visible image
- Display monitor - Shows real-time images
- C-arm - Movable arc positioning source and detector
The Process:
- X-rays pass through the body
- Dense structures (bone) block more radiation
- Soft tissues allow more radiation through
- Differences create contrast on the image
- Continuous imaging shows needle movement
Radiation Considerations
Modern fluoroscopy uses minimal radiation:
- Equivalent to a few X-rays
- Far less than a CT scan
- Considered safe for occasional procedures
- Exposure time is brief (seconds to minutes)
Part 2: Accuracy Data
Research Findings
Multiple peer-reviewed studies have compared blind vs. fluoroscopy-guided injections:
Jackson et al. (JBJS)
- Blind accuracy: 77%
- Fluoroscopy accuracy: 100%
- Confirmation method: Arthroscopy
Berkoff et al. (Clinical Journal of Sport Medicine)
- Blind accuracy: 72%
- Fluoroscopy accuracy: 100%
- Study population: 77 patients
Park et al.
- Blind accuracy: 75%
- Fluoroscopy accuracy: 99%
- Large population study
Where Missed Injections Go
Anatomical analysis of inaccurate injections shows medication deposited in:
| Location | Frequency |
|---|---|
| Hoffa’s fat pad | 35% of misses |
| Suprapatellar bursa | 25% of misses |
| Pes anserine region | 20% of misses |
| Subcutaneous tissue | 15% of misses |
| Other locations | 5% of misses |
Part 3: The Procedure
Pre-Procedure
Patient Preparation:
- No fasting required
- Wear loose, comfortable clothing
- Arrive 15 minutes early
- Bring medication list
- Bring insurance cards
Medical Review:
- Confirm diagnosis and indication
- Review allergies (contrast, medications)
- Check for contraindications
- Verify no blood thinners (if applicable)
Equipment Setup
Room Components:
- Fluoroscopy C-arm unit
- Sterile procedure tray
- Contrast dye (iodinated)
- Local anesthetic
- Treatment medication (HA, steroid)
- Monitoring equipment
Sterile Supplies:
- Antiseptic solution
- Sterile drapes
- Appropriate gauge needles
- Syringes
- Bandages
Step-by-Step Procedure
1. Positioning (2-3 minutes)
- Patient positioned supine or seated
- Knee positioned for optimal access
- C-arm positioned over knee
2. Preparation (3-5 minutes)
- Skin cleaned with antiseptic
- Sterile drape placed
- Local anesthetic administered
- Wait for numbing effect
3. Needle Insertion (5-7 minutes)
- Fluoroscopy activated
- Needle advanced under visualization
- Real-time guidance to joint space
- Approach adjusted as needed
4. Confirmation (1-2 minutes)
- Small amount of contrast injected
- Contrast outlines joint space
- Confirms intra-articular position
- Images saved for documentation
5. Medication Delivery (1-2 minutes)
- Treatment medication injected
- Distribution observed on fluoroscopy
- Needle removed
- Site bandaged
Post-Procedure
Immediate:
- Brief rest (5-10 minutes)
- Ambulate to confirm stability
- Receive aftercare instructions
- Schedule follow-up if needed
Same Day:
- May drive self home
- Resume normal activities
- Ice if minor discomfort
- Avoid strenuous activity for 24-48 hours
Part 4: Contrast Dye
Purpose
Contrast dye (typically iodinated) provides definitive confirmation of needle placement before medication delivery.
How It Works
- Small amount (0.5-1ml) injected through needle
- Contrast appears bright white on fluoroscopy
- If in joint, outlines articular surfaces
- Pattern confirms intra-articular vs. extra-articular
Contrast Patterns
Correct Placement:
- Smooth outline of joint surfaces
- Fills joint space evenly
- No leakage outside joint capsule
Incorrect Placement:
- Irregular distribution
- Remains localized (not spreading)
- Tracks along soft tissue planes
Allergy Considerations
For patients with iodine contrast allergy:
- Pre-medication protocols available
- Alternative contrast agents exist
- Ultrasound guidance can be substituted
- Discuss with provider beforehand
Part 5: Comparison to Other Techniques
Blind (Landmark-Guided)
| Factor | Blind | Fluoroscopy |
|---|---|---|
| Accuracy | 70-80% | 100% |
| Confirmation | Feel only | Visual + contrast |
| Time | 5-10 min | 15-20 min |
| Cost | Lower | Higher (but covered) |
| Equipment | Minimal | Specialized |
Ultrasound-Guided
| Factor | Ultrasound | Fluoroscopy |
|---|---|---|
| Accuracy | 96-100% | 100% |
| Visualization | Soft tissue + needle | Bone + contrast |
| Radiation | None | Minimal |
| Portability | High | Lower |
| Confirmation | Real-time | Contrast definitive |
When Each Is Preferred
Fluoroscopy preferred:
- Obese patients
- Complex anatomy
- Previous surgery
- Need for definitive confirmation
- Calcified or bony landmarks helpful
Ultrasound preferred:
- Radiation concern
- Soft tissue visualization needed
- Portable requirement
- Serial procedures
Part 6: Clinical Outcomes
Pain Relief Comparison
Studies comparing outcomes by guidance method:
| Outcome | Blind | Guided |
|---|---|---|
| Pain reduction | Variable | Consistent |
| Duration of relief | Shorter | Longer |
| Need for repeat | Higher | Lower |
| Patient satisfaction | 60-70% | 85-95% |
Why Accuracy Affects Outcomes
When medication is deposited extra-articularly:
- No direct joint surface coating
- Limited anti-inflammatory effect
- Reduced mechanical lubrication
- Systemic absorption instead of local effect
Long-Term Implications
Accurate treatment allows:
- Proper evaluation of treatment response
- Informed decisions about next steps
- Avoiding premature surgical referral
- Maximizing conservative care window
Part 7: Provider Qualifications
Who Performs Fluoroscopy-Guided Injections
Interventional Pain Management Physicians
- Fellowship-trained in image-guided procedures
- Regular use of fluoroscopy
- High volume of injection procedures
Sports Medicine Physicians
- Often fellowship-trained in musculoskeletal procedures
- May use fluoroscopy or ultrasound
- Focus on athlete and active patient populations
Interventional Radiologists
- Extensive imaging expertise
- May perform joint injections
- Access to full imaging capabilities
Some Orthopedic Surgeons
- Particularly those with sports medicine focus
- Variable use of imaging guidance
- May prefer surgical suite access
Questions to Ask
- “Do you use fluoroscopy guidance for knee injections?”
- “How many guided injections do you perform annually?”
- “Will contrast be used to confirm placement?”
- “Can I see the images during/after the procedure?”
Part 8: Medicare Coverage
Coverage Details
Medicare Part B covers:
- Fluoroscopy guidance (CPT 77002)
- Knee joint injection procedure
- Hyaluronic acid medication
- Contrast material
No Additional Patient Cost
The imaging guidance is included in procedure coverage—patients don’t pay extra for this higher-quality approach.
Documentation Requirements
For coverage:
- Medical necessity established
- Diagnosis code for knee osteoarthritis
- Conservative treatment documented
- Procedure notes with imaging confirmation
Part 9: Safety Profile
Risks of Fluoroscopy-Guided Injection
Minimal Risks:
- Brief radiation exposure (equivalent to 2-3 X-rays)
- Contrast allergy (rare, pre-screening performed)
- Infection (less than 0.1% with sterile technique)
- Bleeding at puncture site (minor)
Serious Complications:
- Extremely rare with proper technique
- No significant difference from blind injection
- Benefits far outweigh minimal risks
Contraindications
Relative contraindications:
- Pregnancy (radiation concern)
- Severe contrast allergy (alternatives available)
- Skin infection at site (delay procedure)
- Uncontrolled bleeding disorder
Summary: Why Fluoroscopy Matters
- 100% accuracy ensures medication reaches the joint
- Contrast confirmation provides definitive proof
- Visual documentation creates permanent record
- Consistent outcomes due to reliable delivery
- Covered by Medicare at no additional cost
For patients with knee osteoarthritis seeking optimal treatment outcomes, imaging-guided injection represents the gold standard in technical accuracy.
Next Steps
Take our Knee Health Score Quiz to assess your candidacy for Medicare-covered, imaging-guided gel therapy.
Found this guide helpful?
Get more in-depth resources delivered to your inbox.
Join 10,000+ readers. No spam.