Shoulder Arthritis vs Rotator Cuff: How to Tell the Difference
Struggling to determine if your shoulder pain is arthritis or a rotator cuff injury? Learn the key differences in symptoms, causes, and treatments to get the right diagnosis.
By Joint Pain Authority Team
Key Takeaways
- Shoulder arthritis and rotator cuff tears can cause similar pain but have distinct differences in motion patterns and symptoms
- Arthritis typically causes pain during all shoulder movements, while rotator cuff tears show weakness with specific motions
- Many people over 60 have both conditions simultaneously, which requires specialized treatment
- Accurate diagnosis through examination and imaging determines the most effective treatment approach
Your shoulder hurts. It’s been hurting for weeks, maybe months. You can’t reach overhead easily, and sleeping on that side is uncomfortable. But what’s actually causing the pain?
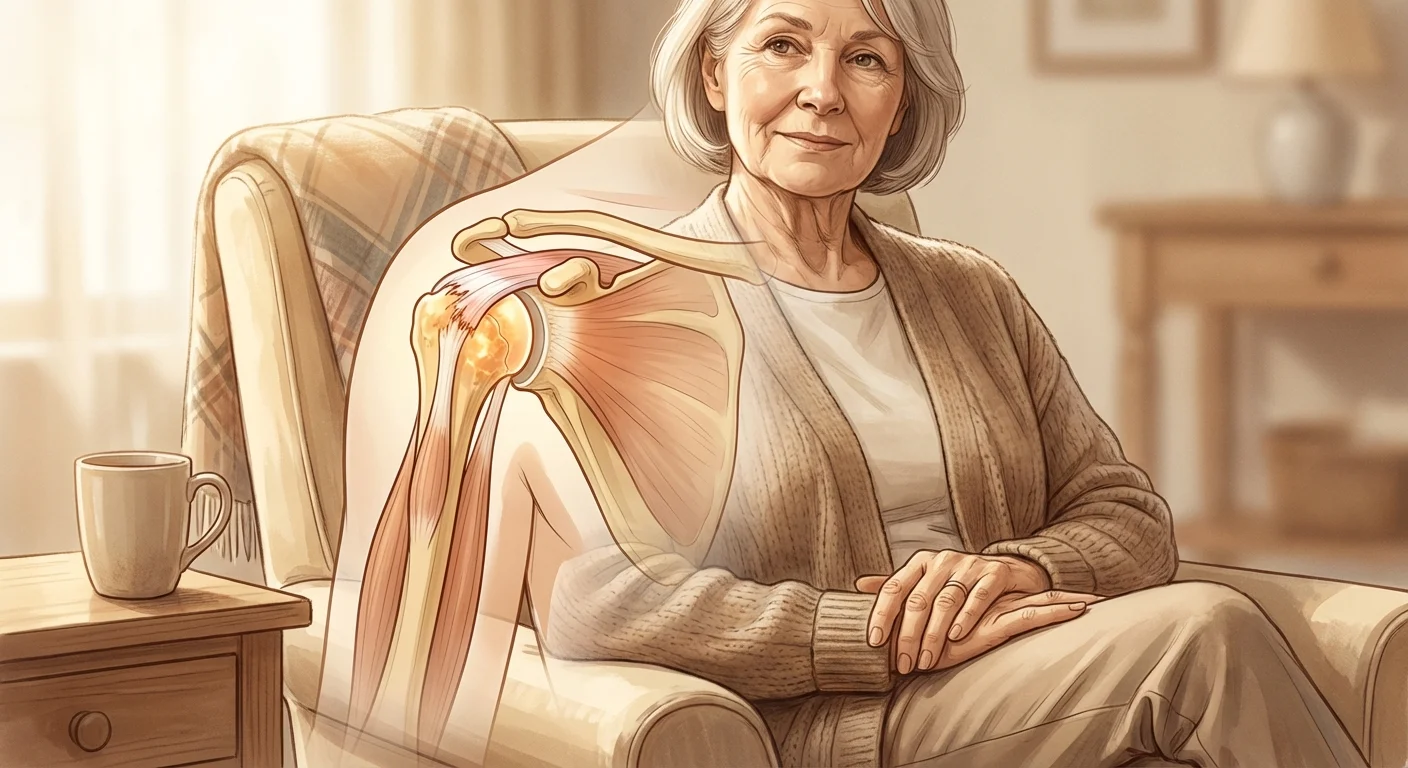
Two of the most common shoulder problems—osteoarthritis and rotator cuff tears—can feel remarkably similar. Both cause pain, both limit your movement, and both become more common after age 50. But they’re fundamentally different conditions that require different treatments.
Understanding the key differences helps you have more informed conversations with your doctor and understand why certain treatments are recommended.
What’s the Basic Difference?
Shoulder Osteoarthritis
Shoulder arthritis is a joint surface problem. The cartilage that covers the bones in your shoulder joint gradually wears away. As the protective cushioning disappears, the bones can rub together, causing pain and inflammation.
Think of it like brake pads wearing down—eventually, metal grinds on metal.
Key feature: The problem is inside the joint itself, affecting the joint surfaces.
Rotator Cuff Tears
A rotator cuff tear is a tendon problem. The tendons that connect muscles to bone become damaged or torn. These tendons control your shoulder’s rotation and stability. When they’re torn, the muscles can’t work properly.
Think of it like a frayed rope that can no longer support the weight it’s designed to hold.
Key feature: The problem is with the soft tissues surrounding the joint, not the joint surface itself.
How Symptoms Differ
While both conditions cause shoulder pain, the pattern and quality of symptoms offer important clues.
Pain Location and Quality
Arthritis Pain:
- Deep, aching pain inside the shoulder joint
- Located at the back and front of the shoulder
- Often described as a “toothache” in the shoulder
- Pain typically consistent across different movements
- May radiate down the arm
Rotator Cuff Pain:
- Pain on the outer aspect of the shoulder
- Radiates down the side of the upper arm (rarely below the elbow)
- Often sharp with certain movements
- Specific movements hurt more than others
- May have a “pinching” sensation
When Pain Occurs
Arthritis:
- Pain during all shoulder movements
- Worse after activity or at end of day
- Weather changes may trigger flares
- Stiffness after periods of inactivity
- Pain relatively consistent in all directions of movement
Rotator Cuff Tear:
- Pain with specific movements (especially raising arm to the side or reaching behind back)
- Night pain is a hallmark symptom—often the worst pain
- Pain when lying on the affected shoulder
- May have pain-free range in certain directions
- Pain often worse with overhead activities
Range of Motion Patterns
This is where the two conditions show the clearest differences.
Arthritis:
- Gradual loss of motion in all directions
- Both active (you moving it) and passive (someone else moving it) motion are limited
- Motion loss is global—rotation, reaching forward, reaching back all affected
- Feels stiff in all directions
Rotator Cuff Tear:
- Weakness with specific movements (lifting arm to side, rotating outward)
- Passive motion (someone else moving your arm) is often better than active motion
- May have full motion in some directions
- Weakness is more prominent than stiffness
Key diagnostic test your doctor will use: If someone else can move your shoulder farther than you can move it yourself, this suggests a rotator cuff problem. If your shoulder is equally limited whether you or someone else moves it, this suggests arthritis.
Strength Differences
Arthritis:
- Strength is relatively preserved until advanced stages
- Weakness comes from pain, not mechanical failure
- Muscles work, but moving hurts
- Can usually hold arm up if you help lift it to that position
Rotator Cuff Tear:
- Weakness is a hallmark symptom
- Difficulty initiating certain movements
- Arm may “drop” when trying to hold it in certain positions
- Weakness out of proportion to pain in some cases
- Specific weakness patterns (can’t lift to the side, can’t rotate outward)
How They Develop
Arthritis Development
Shoulder arthritis usually develops:
- Gradually over many years
- From natural wear and tear (primary osteoarthritis)
- After previous injuries or surgery (post-traumatic arthritis)
- As a consequence of inflammatory arthritis (rheumatoid arthritis)
- Accelerated by rotator cuff tears (rotator cuff tear arthropathy)
Timeline: Symptoms typically worsen slowly over years. You may have years of mild symptoms before they become bothersome.
Rotator Cuff Tear Development
Rotator cuff tears can develop:
- Acutely from a fall, injury, or lifting something heavy
- Degeneratively over time from repetitive motions and aging
- Progressively starting as small tears that gradually enlarge
- From a combination of age-related wear and sudden stress
Timeline: Acute tears cause sudden pain and weakness. Degenerative tears may have a slower onset but often worsen over months rather than years.
Age and Risk Factors
Who Gets Arthritis?
Peak age: 55-80 years old
Major risk factors:
- Previous shoulder injuries or surgery
- Family history of arthritis
- Heavy lifting occupations
- Inflammatory conditions
- Long-standing rotator cuff tears
Who Gets Rotator Cuff Tears?
Peak age: 40-70 years old (but can occur at any age with injury)
Major risk factors:
- Age over 40 (degenerative tears)
- Repetitive overhead motions (painting, construction, swimming, tennis)
- Previous shoulder injuries
- Smoking (reduces blood flow to tendons)
- Family history
Important note: Many people over 60 have both conditions simultaneously.
Diagnostic Tests: What Your Doctor Will Do
Physical Examination
For Arthritis:
- Assess passive and active range of motion (both limited equally)
- Check for grinding or clicking (crepitus)
- Specific tests: Cross-body adduction test, apprehension test
- Evaluate for muscle atrophy (wasting)
For Rotator Cuff:
- Strength testing in specific positions
- Specific tests: Empty can test, drop arm test, external rotation test
- Compare passive vs. active motion (passive better suggests tear)
- Check for muscle atrophy of rotator cuff muscles
Imaging Studies
X-rays:
- Arthritis: Shows joint space narrowing, bone spurs, changes in bone shape
- Rotator Cuff: X-rays are usually normal (shows bone, not soft tissue)
MRI:
- Arthritis: Shows cartilage loss, bone marrow changes, joint effusion
- Rotator Cuff: Clearly shows tendon tears, their size, and tendon quality
Ultrasound:
- Can detect rotator cuff tears
- Limited for viewing arthritis
- Dependent on technician skill
- Less expensive than MRI
Can You Have Both?
Yes—and it’s common after age 60.
When a rotator cuff tear exists for a long time, it can lead to arthritis development. This condition is called rotator cuff tear arthropathy. Here’s why it happens:
- The torn rotator cuff allows the humerus (upper arm bone) to move abnormally in the socket
- This abnormal motion causes uneven stress on the cartilage
- Over months to years, the cartilage breaks down
- Arthritis develops in a joint that already has a rotator cuff tear
If you have both:
- Treatment becomes more complex
- Conservative treatments are tried first
- Surgery options are different (may require reverse shoulder replacement)
- Physical therapy focuses on muscles that still work
- Expectations for recovery may be different
Treatment Approaches: How They Differ
Conservative Treatment
Both conditions benefit from:
- Physical therapy (though with different focuses)
- Anti-inflammatory medications
- Activity modification
- Ice and heat therapy
Arthritis-specific treatments:
- Focus on maintaining range of motion
- Gentle stretching exercises
- Avoiding overuse but staying active
- Weight management (reduces systemic inflammation)
Rotator cuff-specific treatments:
- Strengthening remaining rotator cuff muscles
- Scapular stabilization exercises
- Avoiding overhead strain
- Proper shoulder mechanics training
Injection Therapies
For Arthritis:
- Corticosteroid injections: Reduce inflammation, provide 4-12 weeks of relief
- Hyaluronic acid injections: Emerging evidence for shoulder OA, may provide longer relief
- Goal: Reduce inflammation, improve function
For Rotator Cuff Tears:
- Corticosteroid injections: Help with bursitis and inflammation around the tear
- PRP injections: May promote healing in partial tears (mixed evidence)
- Goal: Reduce pain, improve function, potentially promote healing
Important note: Repeated corticosteroid injections in rotator cuff conditions can weaken the tendon further. Limited use is recommended.
Surgical Options
Arthritis Surgery:
- Arthroscopic debridement: Remove loose cartilage and bone spurs (limited benefit)
- Shoulder replacement: Resurface or replace the joint
- Reverse total shoulder replacement: When rotator cuff is also damaged
Rotator Cuff Surgery:
- Arthroscopic repair: Reattach torn tendon to bone
- Open repair: For large or complex tears
- Superior capsular reconstruction: For massive tears that can’t be repaired
- Debridement only: For tears that can’t be repaired in low-demand patients
When arthritis and rotator cuff tear coexist:
- Reverse total shoulder replacement is often the best option
- This specialized implant design works even without a functioning rotator cuff
- Good pain relief and functional improvement in most cases
Making the Diagnosis: What to Expect
When you see a doctor for shoulder pain, here’s the typical process:
Step 1: History
Your doctor will ask about:
- When the pain started (sudden vs. gradual)
- What makes it better or worse
- Whether you had an injury
- Night pain and sleep disruption
- What activities you can’t do anymore
- Previous shoulder problems
Step 2: Physical Examination
Your doctor will:
- Watch you move your shoulder
- Move your shoulder for you (passive range)
- Test strength in different positions
- Perform specific diagnostic tests
- Feel for tenderness and grinding
Step 3: Imaging
Based on examination findings:
- X-rays first: Rule out arthritis, fractures, bone spurs
- MRI if needed: When rotator cuff tear is suspected or surgery considered
- Ultrasound alternative: In some cases, for rotator cuff evaluation
Step 4: Diagnosis and Treatment Plan
Your doctor will:
- Explain which condition you have (or if you have both)
- Discuss treatment options appropriate for your diagnosis
- Set realistic expectations for recovery
- Create a treatment plan
Real-World Scenarios
Scenario 1: Progressive Stiffness
Maria, 68: “My shoulder has been getting stiffer over the past three years. It hurts to reach overhead and behind my back. The pain is deep inside the shoulder and aches most of the time. I can’t sleep on that side anymore.”
Likely diagnosis: Shoulder osteoarthritis
Key clues: Gradual progression, global stiffness, deep aching pain, symmetrical motion loss
Scenario 2: Sudden Weakness
Robert, 58: “I was lifting something heavy three months ago and felt a pop. Since then, I can’t lift my arm to the side without pain. It’s especially bad at night. Someone else can move my arm higher than I can move it myself.”
Likely diagnosis: Rotator cuff tear
Key clues: Specific inciting event, weakness with specific motion, night pain, discrepancy between active and passive motion
Scenario 3: Both Conditions
Linda, 72: “I’ve had shoulder arthritis for years, but over the past six months, my shoulder has gotten much weaker. I’m having trouble lifting my arm, and the pain is worse than it’s ever been.”
Likely diagnosis: Rotator cuff tear arthropathy (both conditions)
Key clues: Pre-existing arthritis, new onset weakness, rapid worsening of symptoms
Questions to Ask Your Doctor
- Do I have arthritis, a rotator cuff tear, or both?
- If I have a rotator cuff tear, how large is it and which tendon(s) are involved?
- Is my rotator cuff tear likely to get worse without surgery?
- If I have arthritis, how advanced is it?
- What are my treatment options given my specific diagnosis?
- How do we decide between conservative treatment and surgery?
- If I need surgery eventually, what are the benefits of trying other treatments first?
- What activities should I avoid to prevent worsening?
The Bottom Line
Shoulder arthritis and rotator cuff tears are different conditions that can feel similar but require different approaches:
Shoulder Arthritis:
- Joint surface problem
- Global stiffness in all directions
- Deep, aching pain
- Strength relatively preserved
- Develops gradually over years
Rotator Cuff Tears:
- Tendon problem
- Specific weakness patterns
- Night pain common
- Passive motion better than active
- Can develop suddenly or gradually
Many people over 60 have both, which makes treatment more complex. Accurate diagnosis through examination and imaging is essential to choosing the right treatment.
If you’re experiencing shoulder pain, don’t assume you know what’s causing it. See a shoulder specialist for a proper evaluation. The good news is that both conditions have effective treatments when diagnosed correctly.
Related Resources
Enjoyed this article?
Get more insights like this delivered to your inbox weekly.
Join 10,000+ readers. No spam.